
Overview
- Tyrosinemia is one type of amino acid disorder
- It is a genetic disorder characterized by disruptions in the multistep process that breaks down the amino acidtyrosine, a building block of most proteins. If untreated, tyrosine and its byproducts build up in tissues and organs, which can lead to serious health problems.
- There are three types of tyrosinemia, which are each distinguished by their symptoms and genetic cause. Tyrosinemiatype I, the most severe form of this disorder, is characterized by signs and symptoms that begin in the first few months of life.
Prevalence:
Worldwide, tyrosinemia type I affects about 1 in 100,000 individuals. This type is more common in Norway where 1 in 60,000 to 74,000 individuals are affected. Tyrosinemia type I is even more common in Quebec, Canada where it occurs in about 1 in 16,000 individuals (Genetics Home Reference).
- In Pakistan this disorder is less documented and still in study.
Causes:
Tyrosinemia is caused by mutations in the fumarylacetoacetate hydrolase (FAH) gene that is responsible for the production of the FAH enzyme. Deficiency of this enzyme leads to an accumulation of fumarylacetoacetate and accumulation of tyrosine and its metabolites in the liver, kidney, and central nervous system eventually causing tyrosinemia type I.
Inheritance:
- Tyrosinemia type I is inherited as an Autosomal recessive genetic condition.
- Recessive genetic disorders results when an individual inherits two copies of an abnormal gene for the same trait, one from each parent. If an individual receives one normal gene and one gene for the disease, the person will be a carrier for the disease but usually will not show symptoms. The risk for two carrier parents to both pass the defective gene and have an affected child is 25% with each pregnancy. The risk to have a child who is a carrier like the parents is 50% with each pregnancy. The chance for a child to receive normal genes from both parents and be genetically normal for that particular trait is 25%. The risk is the same for males and females.
Parents who are close relatives (consanguineous) have a higher chance than unrelated parents to both carry the same abnormal gene, which increases the risk to have children with a recessive genetic disorder.
Clinical Features:
Tyrosinemia 1 in infants (“Acute form”)
Some of the first symptoms may be:
- diarrhea and bloody stools
- vomiting
- poor weight gain
- extreme sleepiness
- irritability
Liver problems are common. They can lead to:
- enlarged liver
- yellowing of the skin
- tendency to bleed and bruise easily
- swelling of the legs and abdomen
Kidney problems also happen and can lead to:
- rickets, a bone thinning condition
- delays in walking
Some babies also have episodes that include:
- pain or weakness, especially in the legs
- breathing problems
- rapid heartbeat
- seizures
- coma, sometimes leading to death
Tyrosinemia 1 in children (“chronic” form):
Children with the chronic form usually start having symptoms after two months of age. Some of the first signs may be trouble gaining weight and episodes of vomiting and diarrhea. Over time, the condition can cause liver, kidney and nerve problems.
Diagnosis:
Screening Method:
Primary newborn screening for tyrosinemia type 1 utilizes tandem mass spectrometry to determine the levels of Succinylacetone (SUAC). Elevated SUAC indicates the possibility of tyrosinemia type 1.
If a baby has a presumptive positive tyrosinemia type 1 newborn screening result, additional testing needs to be performed to confirm a diagnosis.
Follow-up Testing after Positive Screen:
- Quantitative plasma amino acid analysis in an early stage shows selective increases of tyrosine and methionine levels. As hepatic failure progress, levels of most of the other amino acids become elevated.
- Urine organic acid analysis may reveal increased succinylacetone in tyrosinemia I.
- Plasma Amino acid analysis and Urine organic acid analysis is available in AFIP (Armed Force Institute of Pathology) Excel lab, Islamabad Diagnostic Centre and Agha Khan Laboratory.
- DNA testing needs to be obtained for definitive diagnostic confirmation.
Treatment:
Treatment consists of a diet low in tyrosine and phenylalanine and use of a drug (nitisone or NTBC) that prevent formation of succinylacetone, the toxic agent responsible for liver and kidney damage.
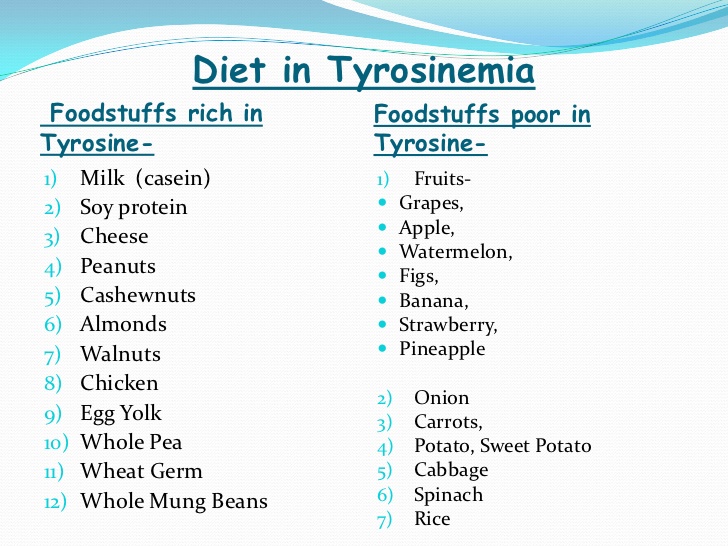
Low-tyrosine / phenylalanine diet:
The diet is made up of foods that are very low in tyrosine and phenylalanine. This means a child will need to limit foods such as cow’s milk and regular formula. He or she will need to avoid meat, eggs and cheese. Regular flour, dried beans, nuts and peanut butter contain these amino acids and must also be limited.
Metabolic doctor and dietician decide on the best food plan for child. The exact plan depends on many things such as child’s age, weight, general health, and how well the medication is working.
With treatment: >90% survival rate can be expected, along with normal growth, normalization of liver function and prevention of cirrhosis, correction of renal tubular acidosis and resolution of secondary rickets. Early treatment is associated with reduced incidence of hepatic cancer.
Without Treatment: chronic problems ensue, including: liver disease leading to cirrhosis and hepatocellular carcinoma, renal tubular disease (Fanconi syndrome), rickets, failure to thrive, and coagulation disorders. Repeated neurologic crises may occur involving mental status change, abdominal pain, peripheral neuropathy, and/or respiratory failure. These are due to the accumulation of delta amino levulinic acid whose metabolism is inhibited by succinylacetone.
References:
- Tyrosinemia: Genetics Home Reference
- Bijarnia S, Puri RD, Ruel J, et al. Tyrosinemia type I–diagnostic issues and prenatal diagnosis. Indian J Pediatr. 2006 Feb. 73(2):163-5.
- Grompe M, St-Louis M, Demers SI, al-Dhalimy M, Leclerc B, Tanguay RM (1994). “A single mutation of the fumarylacetoacetate hydrolase gene in French Canadians with hereditary tyrosinemia type I”. N. Engl. J. Med. 331(6): 353–7. PMID 8028615. doi :1056/NEJM199408113310603.
- Masurel-Paulet A, Poggi-Bach J, Rolland MO, et al. NTBC treatment in tyrosinaemia type 1: long-term outcome in French patients. J Inherit Metab Dis. 2008; 31: 81-7.
- McKiernan PKJ. Nitisinone in the treatment of hereditary tyrosinaemia type 1. Drugs. 2006; 66: 743-50.
Leave a Reply